Cells serve as the body’s social network, communicating with each other through the transmission of extracellular vesicles – tiny membrane-bound messages in a bottle. The study of EVs is rapidly expanding across various scientific disciplines worldwide, as researchers explore their potential use in medical diagnostics and therapy. Numerous studies have already investigated the use of EVs in a broad range of applications, including cancer diagnosis and treatment, as well as wrinkle reduction.
A recently published study co-authored by a researcher at The University of North Texas Health Science Center at Fort Worth, which houses The North Texas Eye Research Institute, focuses on EVs.
Dr. Dimitrios Karamichos has conducted research on the correlation between keratoconus, an eye disease, and EVs found in tears. Karamichos and his team have successfully identified, isolated, and characterized tear EVs in individuals affected by the disease. This research has the potential to uncover the root cause of the debilitating eye condition and provide effective treatment options.
Karamichos, who serves as the executive director of the Eye Institute, believes that this study is just the beginning of a vast and unexplored area of research related to keratoconus. He hopes that by understanding the role of EVs in the disease, new drug development and therapeutic options can be developed to improve the lives of those suffering from this condition.
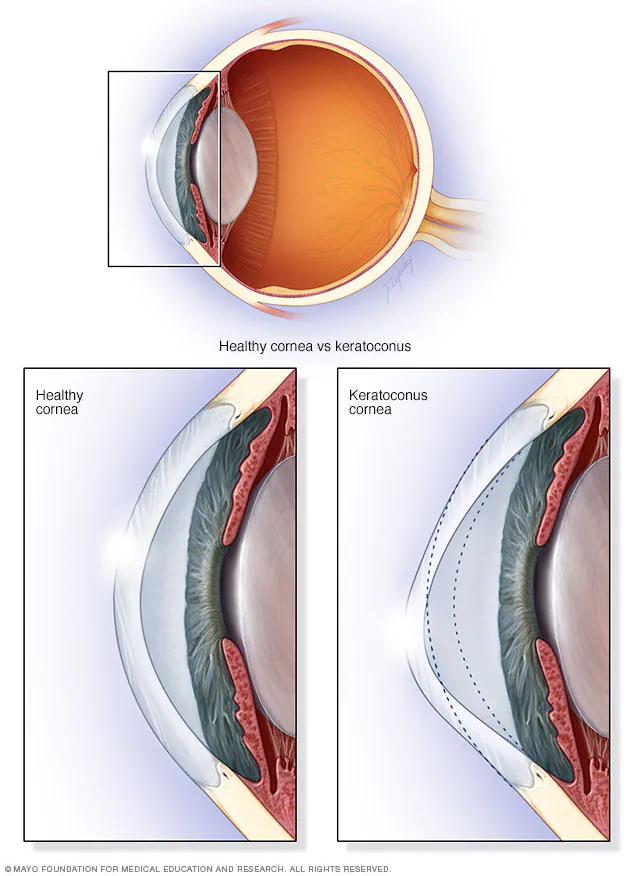
What is Keratoconus?
Keratoconus is a condition where the cornea, which is the clear, dome-shaped front surface of the eye, thins and gradually bulges outward into a cone shape. This can result in blurry and distorted vision. In severe cases, it can lead to corneal scarring, which greatly diminishes vision and can even cause blindness.
The exact cause of keratoconus is unknown, but most researchers believe it is a combination of genetics, hormonal imbalances, and environmental factors such as allergies and eye rubbing. It typically occurs in late childhood or early adulthood and stabilizes around ages 40 to 45. In severe cases, a corneal transplant may be necessary.
Karamichos is a leading researcher on keratoconus. He has conducted studies and published research on a predictive biomarker for the disease, the effects of certain hormones that cause keratoconus, and the link between people with Down syndrome and the condition.
More About Extracellular Vesicles (EVs)
In his latest study, the Greek-born researcher and his co-investigators discovered that tear extracellular vesicles (EVs) have a distinct phenotype compared to their healthier counterparts. The research team also concluded that tear EVs from male subjects showed higher total counts, which could be significant as more data emerges.
To conduct their research, the team examined tears in the lateral meniscus of ten healthy subjects (five males and five females) and nine individuals diagnosed with keratoconus (four males and five females).
“Keratoconus is an unpredictable, multifactorial disease that causes vision problems for many people,” Karamichos said. “With corneal transplants as the gold standard for treating severe keratoconus, the field is in need of non-invasive, personalized solutions and treatments. My research has always been driven by the needs of clinics, as I strive to make my discoveries applicable to the real world.”
Tear EVs have been linked to other conditions, such as dry eye, Sjogren’s Syndrome, and types of glaucoma. With his latest work, Karamichos is bringing his life’s work to this new research frontier.
“Extracellular vesicles and related studies have exploded in the ophthalmology world over the last five years or so,” he said. “EVs seem to be so powerful, carrying all sorts of important information (DNA, miRNAs) over long distances within the body. Yet, we know very little about them in the context of corneal health.”
“Keratoconus disease and the status of the tear film are intimately connected, but it is not clear at this point what component within the tear fluid contributes to the pathobiology of the disease,” he continued. “Curiosity and the potential for clinical applicability led me to initiate this research.”